Cavernoma
Make an Appointment
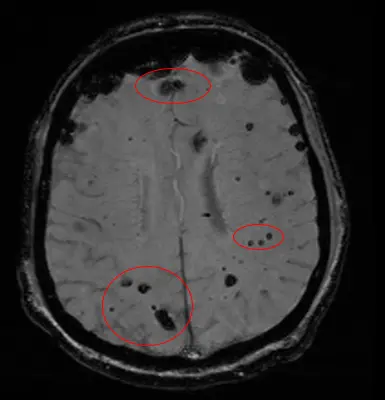
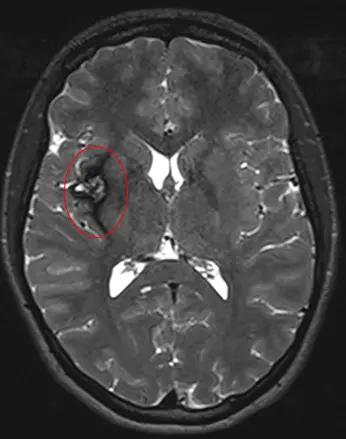
Cavernomas are enlarged and deformed blood vessels gathered into clusters. These clusters, called angiomas, may look bubbly, like raspberries. A cavernoma can appear in the brain, spinal cord or other parts of the nervous system and body, including on the skin and eye.
Cavernomas can cause:
- Leaking blood
- Arm or leg weakness
- Damaged vision, balance, memory, or attention
- Stroke in younger people
Cavernoma Center of Excellence
We're recognized as a Center of Excellence by the Angioma Alliance — one of only eight around the country, and the only one found in the Southeast region.
We've received this designation not only because of the high-quality care delivered by our dedicated team. Centers of Excellence also research new technologies and techniques for treating cavernomas.
Types of Cavernomas
Cavernomas come in two forms:
- Sporadic — most common; when only one cavernoma develops, and the condition doesn’t run in your family
- Familial — less common; more than one cavernoma occurs and the condition runs in your family
Other terms used for this condition includes cerebral cavernous malformations (CCMs), cavernous angiomas, or cavernous hemangiomas.
Enlarged Blood Vessel Clusters in the Brain
Cerebral cavernous malformations, or CCMs, are abnormal blood vessels that gather into clusters about the size of a raspberry.
ANDREW SOUTHERLAND: CCM stands for Cerebral Cavernous malformations. These are vascular malformations that occur in the brain. In some folks, they can be sporadic, meaning that there's no tendency for them to run in families. In other patients, it can be genetic, meaning that they do run in families. What they are specifically are little malformations of blood vessels in the brain that are not attached to the normal circulation of the brain. Oftentimes, we find them incidentally and we have to keep an eye on them and they don't cause patients many problems. But in other cases, they can be a source for stroke, meaning on the brain or even seizures in folks that have epilepsy related to cavernous malformations.
ZUSEEN RANNIGAN: The primary symptom per say for patients who have CCM is seizures So patients who have seizures sometimes get worked up and then discover that they had CCM. Other than that, there really isn't a warning sign aside from having an actual bleed which may result in severe neurological deficits whether that be facial droop, extremity weakness, that sort of thing.
ANDREW SOUTHERLAND: We will assess the location of the cavernous malformation, we'll try to use some advanced imaging such as MRI based imaging to see if there's been any prior bleeding or swelling around the cavernous malformation that might give us a sense of its risk for future complications. And then we may make a decision ranging from we're just going to keep an eye on it with some monitoring with imaging over time on some sort of regular basis depending on the patient and the patient's family history and genetic profile. We may refer them for genetic counseling.
CHELSEA CHAMBERS: About 80 percent of the time they're sporadic but the 20 percent of the time when they're familial is when I become involved and that means that there could be an underlying genetic reason behind them.
BARRETT ZLOTOFF: What is a dermatologist doing on the CCM team? Because this is a disease of the brain. What we've discovered is that there are lesions in other organs as well. And one of the main places where there are lesions is in the skin. So 30 percent of patients with CCM will have skin lesions.
ANDREW SOUTHERLAND: UVA is the first health system in the Commonwealth of Virginia to be an HMO Licensed Clinical Center for the management of patients with cavernous malformations. And so we are fortunate to have that designation because of the comprehensive approach we take to the management of patients with cavernous malformations.
ZUSEEN RANNIGAN: We have dedicated our practice to wanting to provide the best, safest and most thorough care for CCM patients.
Cavernoma Treatment at UVA
Our treatment team includes neurologists, neurosurgeons, skin specialists, imaging specialists, and genetic counselors. Together, we develop a strategy to address your cavernoma symptoms.
Treating a Cavernoma
Cavernomas are diagnosed using magnetic resonance imaging (MRI). Treatment for cavernomas includes:
- Medication — If you are having seizures, you may be given medications to stop them.
- Surgery — You may need surgery to remove your cavernoma if you're experiencing symptoms.
- Genetic testing and counseling — If cavernomas run in your family, we may be able to identify the affected genes. We may also be able to determine if you have family members with the affected gene.
Most cavernomas do not need surgery. If you aren’t having symptoms, your healthcare provider will use MRI to monitor for any changes in your cavernoma.
How Do I Know if I Have a Cavernoma?
Usually, you won’t know until the cavernoma causes a seizure. Sometimes they are found when you get brain imaging for other reasons. Symptoms generally appear when cavernomas bleed, and they may include:
- Seizure
- Sudden headache
- Nausea and/or vomiting
- Weakness or numbness on one side of the body
- Difficulty speaking or understanding speech
- Double vision or loss of vision
- Balance problems
Cavernomas on the skin are often seen in cases of familial cavernoma. They usually appear on your arms or legs, and have the same bubbly, berry-like appearance.
What Should I Bring to My Appointment?
For your first appointment, you should bring any previous brain imaging, like MRIs or CT scans, with you.
If you can, you should also ask your biological parent(s) the following questions, and bring the answers with you:
- Have you been diagnosed with a cavernoma?
- Have you ever had seizures?
- Have you ever had a stroke?
- Do you have a history of headaches?
- Do you have siblings (brothers and sisters)? If so, do they have a history of seizures, headaches or strokes?
- Do you know where your ancestors came from?
Patient Resources
Check out the Angioma Alliance for more information and resources about both sporadic and familial cavernomas.